Back in July, we brought you Part I of a series of posts about how to afford Sovaldi (sofosbuvir), the new Hepatitis C (Hep C) cure in the form of a $1,000 pill — $84,000 for the standard 12-week treatment. We focused on consumers paying for Sovaldi in cash. It wasn’t pretty.
Thankfully, most Americans who are taking and will take Sovaldi are covered by health insurance. And if Sovaldi is on the drug list of your health insurance plan then the cost can be a co-pay of $75/month or sometimes $175/month, which is not too bad all things considered. However, as we know – health insurance policies don’t cover all medications, even ones that are far less expensive than Sovaldi. Not surprisingly, health insurance companies are resisting open coverage policies for Sovaldi. In fact, there’s a big battle brewing between Big Health and Big Pharma about who is to blame for problems with affordable access to Sovaldi and other specialty meds – but that’s for another day.
The short answer to the blog title question is – Sovaldi coverage depends on multiple and often technical variables, such as, your age, current health, efficacy of other treatments, intolerance to treatments that are recommended to be taken with Sovaldi, Hep C genotype, history of drug abuse, and more! Herein I do my best to shed some light on what’s up. I believe you’ll find below that most privately insured Americans with Hep C are not guaranteed access to Sovaldi.
First things first: If your healthcare provider has prescribed Sovaldi for you, then you need to know – does your health insurance currently cover Sovaldi? There are about 40 health insurance companies in the U.S. offering thousands of different insurance plans. In turn, those insurers work with several pharmacy benefit management companies (although there are three big ones) who offer a variety of different benefits. To cull through all health insurance and pharmacy benefit plans for their specific criteria for Sovaldi coverage is beyond the scope of this blog post, and perhaps my skill set, but I have a good idea of what you can expect.
Generally, most private health insurance companies will include Sovaldi on their lists of covered medications, but the drug’s name will be followed by a superscripted character (i.e. *, !, 1). That superscripted character leads you to a phrase that reads PRIOR AUTHORIZATION.
The phrase “prior authorization” annoys me. Once a doctor or other licensed practitioner has prescribed a drug to a patient it should just be covered, accessible and affordable! Prior authorization really means this drug is not covered unless you meet certain criteria.
So what are the requirements that a patient must meet to actually receive coverage by their health insurer for Sovaldi. Below is a list of some requirements that I found in a report by the Institute for Clinical and Economic Review. The following insurers employ some but not all of these requirements – and those with hyperlinks appear most transparent about their specific polices: Health Net, Anthem/Express Scripts, Aetna, CVS/Caremark, and Humana.
1. The patient must be at least 18 years of age.
2. The patient must have a diagnosis of chronic hepatitis C with compensated liver disease.
3. Liver biopsy showing fibrosis corresponding to a Metavir score of greater than or equal to 2 or Ishak score of greater than or equal to 3 or other accepted test demonstrating liver fibrosis.
4. Absence of renal impairment: eGFR must be > 30mL/min/1.73m2.
5. Absence of end stage renal disease (ESRD).
6. A planned course of treatment is documented in medical record.
7. The patient verbally or in writing commits to the documented planned course of treatment including anticipated blood tests and visits, during and after treatment.
8. Neither the patient nor the partner of the patient is pregnant.
9. If patient or their partner is of child bearing age, the patient has been or will be instructed to practice effective contraception during therapy and for 6 months after stopping ribavirin therapy.
Unless you are a healthcare professional (one who knows about Hep C), or have Hepatitis C, then some of the requirements will not be understandable. Here are some generalities. Clearly you have to be an adult, which is not an obstacle to coverage since almost all people with Hep C are adults you have to agree to the treatment in writing; and you can’t be pregnant. Those are straightforward.
Those requirements also tell us that people with Hep C, but healthy livers won’t be covered. In other words, if you have Hep C but your liver is ok (as in Metavir score that is lower than equal to 2, or Ishak score that is lower than 3), you will likely be refused prior authorization. Since most people with Hep C are symptom free, 60% to 70% according to the U.S. Centers for Disease Control and Prevention , most people with Hep C will not be covered for Sovaldi for the foreseeable future.
Sovaldi is not a monotherapy, meaning it’s prescribed with other drugs to treat Hep C. The other treatments are usually, but not only, peginterferon alfa (PEG) and ribavirin (RBV). The treatment combination is also dependent on the Hep C genotype of the patient. There are six genotypes of Hep C: the most common is genotype 1 (80% of people with Hep C), followed by 2 and 3. Clinical guidelines call for most people with genotype 1 to be treated with Sovaldi, PEG and RBV, whereas those with genotype 2 and 3 are prescribed only Sovaldi and RBV. Genotypes 4-6 are exceedingly rare.
Tolerance to PEG is also a common prior authorization factor. One really groundbreaking aspect of the drug is that Sovaldi is an interferon‐free option for patients who are intolerant to interferon, which was once the standard of care before new generation treatments hit the market. For people with genotype 1 who are PEG (interferon)-intolerant, some health insurance companies will prescribe Sovaldi with Oylsio (simeprevir) – yet another treatment for Hep C.
Finally, another factor for insurers is whether or not a patient has a history of illicit drug or alcohol abuse. Some insurers will not cover Sovaldi for people in those categories. Others will only cover people who have not used illegal drugs for six months or more. The rationale for refusing to cover Sovaldi for such patients is not due to known contraindications between Sovaldi and illicit drugs, but because insurers believe that drug abusers will not take their medications as prescribed; failing to follow prescription instructions vastly diminishes the efficacy of Sovaldi – and health insurance companies don’t want to waste money on the drug when it won’t work. As Ed Silverman from Pharmalot reports, some are questioning the ethics of not covering people with substance abuse problems, particularly because a large segment of the Hep C population are known to have substance abuse problems!
As you can see, this is insanely complicated! But how might this all play out in reality?
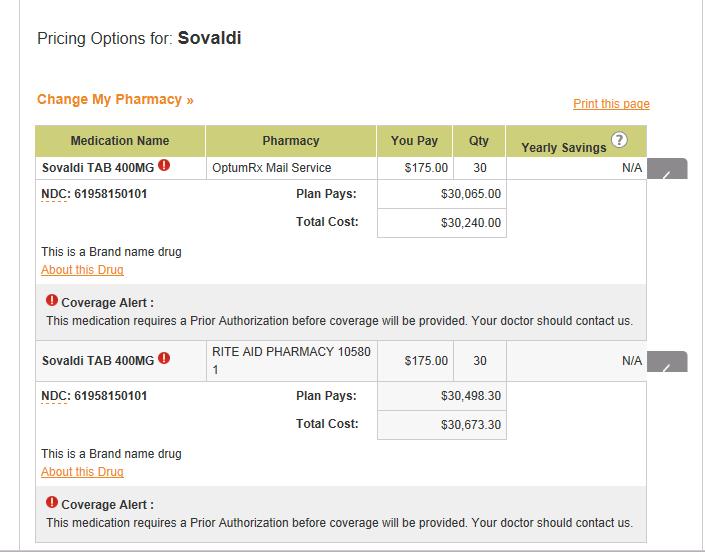
Starting with the lowest hanging fruit I inquired with United Healthcare/Oxford — my own insurance company: here’s what I found. First, my pharmacy benefit manager is a company called OptumRx. I called and spoke with a friendly representative who told me the co-pay would be only $75/month. A great bargain for a drug costing more than $30,000/month! When I checked the website I discovered a discrepancy in what I heard and saw, as per the below chart – but it may have been a miscommunication:
You can see that the co-pay is $175/month, which is still amazing (at least for the patient). For the 12-week course, the patient’s cost would be only $450. But wait, what’s this Coverage Alert? Did you notice the superscript exclamation point in red? It means that you have to obtain prior authorization!
Tagged with: gentotype, prior authorization, sofosbuvir, Sovaldi


To whom it may concern.
My Dr has prescribed Hep C treatment for me. I have Type 2. And my metavir score is between 1.5 and 1.75. Also I have some liver damage.
I am 67 years old and had exposure to Hep earlier in my life as a child and again as a young adult in my late twenties. When my Dr told me I had this condition she recommend that I no longer drink alcohol and refrain from consuming red meat. These I have done.
I am covered through company sponsored Aetna health care. It has been a month since my Dr requested my Rx from the insurance company.
After having read this blog posting I am concerned about my chances of get the prior authorization. Can you direct me to additional resources that may assist me in getting information on how to communicate with and get a resolution from my insurance company??
If I am denied coverage at this time I find it hard to believe that I need to get sicker to get medicine to get better. So without getting too carried away with the negative I would like to know more about resources.
Thanks for your time.
This is America. Where all people are to be treated equally. So why is it that only the rich will receive the newer, more expensive medications like Sovaldi and Harvoni. Its absolutely ludacriss that just because I cant afford to pay $1,000 a day for a pill that will save my life, that I will be left out, to suffer and die. But Im an American!! How can this be? Why doesnt a pharma company, based in the U.S. make this medication and sell it at an affordable price? They could call it “Solve-it-all”
Ummaybe vote for Bernie Sanders… but it think its too late now… le sigh’
Ridiculous in my opinion… Seems “OHP” or my State’s Health Insurance for those of ‘lower income’ aren’t given ANY choice(s) in this nor given an option. After being diagnosed w/Cirrhosis and HCV,along with numerous other issues healt-wise, it’s taken 3 1/2 yrs to regain needed weight and get healthy enough TO tolerate any treatment. The Harvoni I was hoping to acquire and is covered by OHP, isn’t the correct medication for my specific HCV Geno-Type. There’s only 1 other combined w/Ribvarin and one recently newer med that is sadly unobtainable and extremely expensive. The manufacturers of these meds will sometimes assist patients w/the expense of treatment, however not for this specific Rx of Solvaldi and Ribvarin… Kindly kick the low income HCV folks to the curb and let the dog lie dead in the ditch without nary a blink. Guess this is America’s way of weeding out the “unworthy, unwealthy and weak” …along with our elderly communities and the gradual decline of available Social Security matter…I had just gotten healthy enough to consider treatment for the HCV, whereas initially, I felt it was pointless since diagnosed as “terminal” anyway…then I changed my outlook and decided to pursue it …a hopeful possible “remissive cure” that could grant me additional time inwhich to LIVE. …Isn’t going to happen now. Thanks America, Uncle Same and the Corportate Insurance world. You, sorry to say, sadly disappoint and discourage those of us who actually have a need and desire to be and live as healthy as we can, for as long as we can. Something definitely needs to change…Medications are so outragously expensive no matter what the patients diagnosis is, even a mere allergy, for many is unobtainable. That’s just wrong.